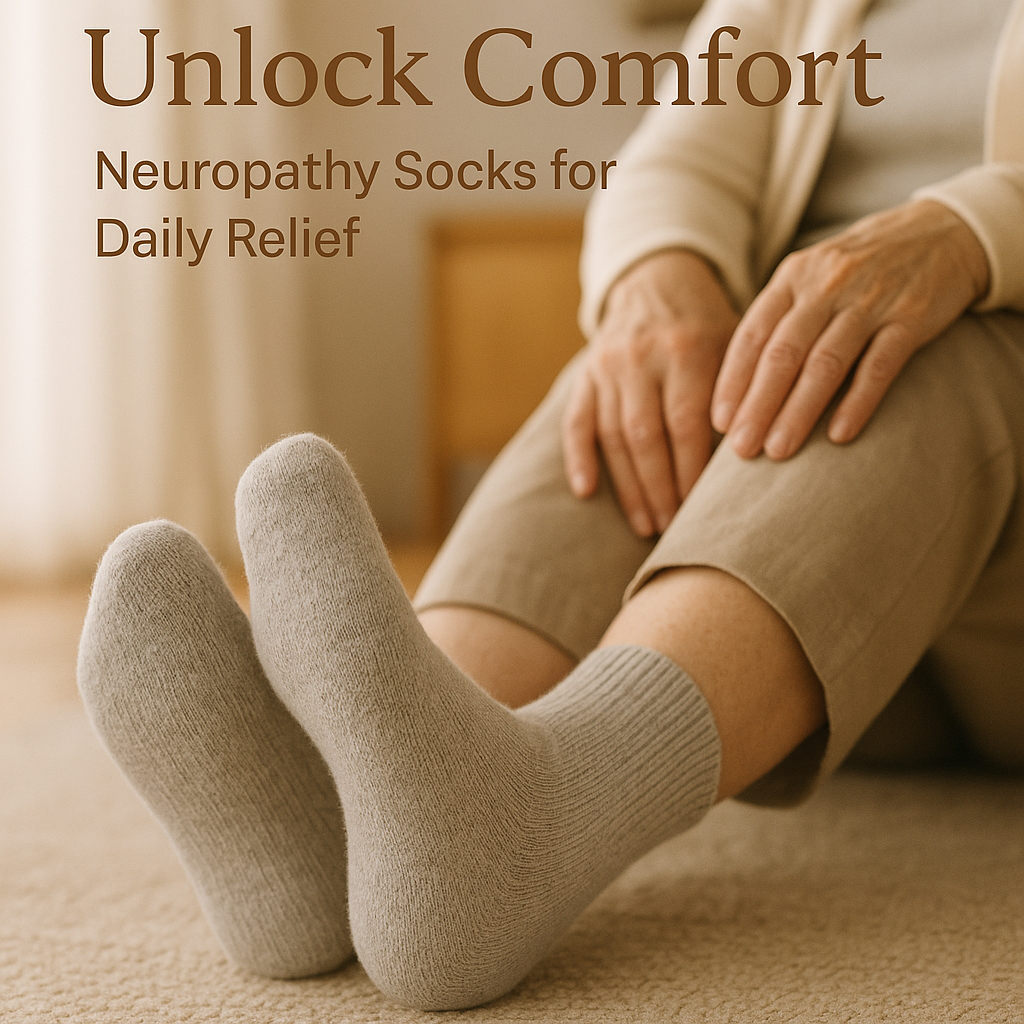
Unlock Comfort: How Neuropathy Socks Can Transform Daily Life for Nerve Pain SufferersUnlock Comfort: How Neuropathy Socks Can Transform Daily Life for Nerve Pain Sufferers
Discover how neuropathy disrupts daily life and why choosing the right neuropathy and compression socks can ease pain and improve mobility. [...]